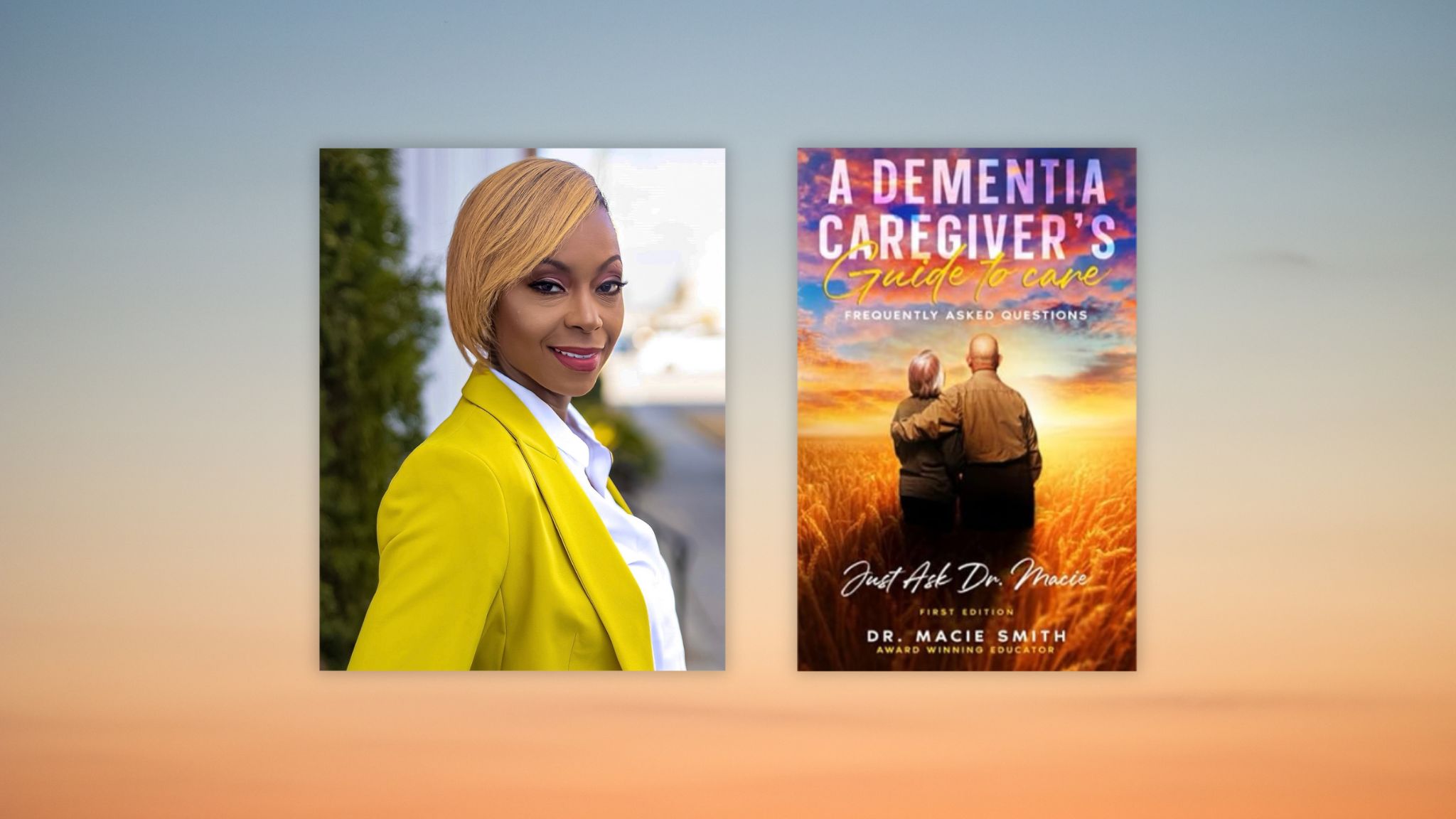
A Dementia Caregiver’s Guide to Care by Macie Smith
Her mission became clear when her grandmother was diagnosed with Alzheimer’s related dementia. “It was one of the scariest times of my life,” says Dr. Macie P. Smith. “I truly did not know what to do or who to call.”
Dr. Smith probably didn’t realize it at the time, but she had suddenly become part of a riveting statistic: While 1.3 million Americans in 2010 needed caregivers or nursing home care, that number is projected to jump to 2.3 million in 2030. The number of Americans living with Alzheimer’s disease is expected to skyrocket to about 14 million by 2050.
In A Dementia Caregiver’s Guide to Care, Dr. Smith hopes to help those who are otherwise unequipped and unprepared to help loved ones stricken with this condition. We got a chance to ask her more about this necessary, meaningful project and what she thinks caregivers need to know in order to aid their loved ones.
Q: Why did you write this book?
A: The market guided my desire to write this book, so to say. My grandmother developed dementia years after I started doing community dementia education and I would share my experiences with my grandma and clients to audiences and they would come back over and over again to hear the same stories because of the practicality of the information and strategies shared. I actually felt terrible that they had to come back to my talks over and over again when I knew they had other priorities, such as taking care of their loved ones. So, I decided to eliminate what could be an inconvenience to accessing tangible information by writing this book.
Q: How well equipped and prepared would you say are today’s typical geriatric caregivers?
A: I would say there is a need for more education and training for caregivers, especially those caring for seniors. The reality is, there are so many caregivers that do not have access to reliable dementia information and resources due to a myriad of reasons (cost, geographical location, health literacy, etc). So, they typically learn how to do things or not do things based on the experience they have working and caring for seniors. Sometimes it works; sometimes it doesn’t.
It is incumbent of our state leaders to make quality, best practice training mandatory for anyone providing care to seniors and those living with dementia, to include a competency-based tool to assess knowledge and retention; and I’m not talking about just an online video or an FAQ sheet that requires a signature. And make these training opportunities available to family members, as well, because it is a team effort when providing care.
Q: What are some of the biggest challenges they face — and are there any pat answers of how to deal with those challenges?
A: One of the biggest challenges faced by family caregivers is the lack of financial resources to secure long term care and support. The other challenge is not having access to reliable, culturally competent, and easy to understand information to help families better manage the impact of behaviors that may present challenges. Caring for someone with dementia is not an individual responsibility, it is a family responsibility; therefore, it’s important that we support the caregivers as well as the person living with the condition. There are some resources out there, but not nearly enough. And the ones that are out there; many families don’t know about them. So, I highly encourage anyone who’s providing care for a senior and/or someone living with dementia to reach out to their local area agency on aging and their local Alzheimer’s Association. Both have respite options and other resources available to support caregivers better understand how to provide care while also providing financial support for that care.
Q: Do you see any common mistakes that caregivers typically make?
A: One of the most common mistakes caregivers make, more often than not, is focusing on the person’s behaviors as opposed to the reasons behind the behaviors and their emotions while the behaviors are happening. Caregivers might get upset when the person gets agitated when he/she can’t remember how to complete a simple task. And instead of caregivers assisting them complete the task and/or offer comfort during this time of frustration, they get frustrated, too, and add more stress to an already stressful situation.
One of the tips I would share when frustrating situations present, is for the caregiver to breathe and take a step back and start all over again when they are calm and not distracted. Those living with dementia are very sensitive to non-verbal cues and will react and respond to caregivers’ emotional state.
Q: Tell us about the solutions you offer in your book. Are there one or two that might seem unusual but truly work?
A: Oh wow, this is a fun question. When it comes to seniors not wanting to drink water, try watering down favorite drinks that might not be as good for the person both physically and/or emotionally, such as soda or alcoholic beverages; for some reason they love … soda. Lol. Also, here’s a tip that’s not in the book (you can thank me later). Put certain drinks in certain cups so that they can identify with the beverage and may be able to make a decision to drink on their own without any reminders or coaching. Think about what cup you use to drink your coffee and what cup you use to drink water. I know you don’t want your coffee in your water cup or your water in your coffee cup, because nothing will go right that day, will it? Lol. So, the same way you identify with what you drink as it relates to your special cups, it applies to those living with dementia, as well.
Q: How do medications factor into treatments?
A: In my professional opinion, medications are a reasonable potential solution for treatment of dementia when all other possible solutions have been tried and tested. I talk about this in my book in terms of treatment for the disease that causes dementia. Right now, Alzheimer’s disease, for example, is not 100% treatable, preventable or curable. However, there are medications out there to treat the symptoms of the disease, dementia.
Now, there are other medications that are prescribed for other things that may or may not be related to dementia, such as agitation and anxiety; however, those medications should be considered with the person’s primary physician and neurologist to assess the benefits and risks. Medications prescribed to those living with dementia that are typically used to treat behavioral health conditions, such as psychosis and schizophrenia (to name a few) are not recommended for seniors and those living with dementia, as it increases their risk for falls, stroke and even death.
Q: Do you have any overall message for today’s geriatric caregivers that you’d like to pass on?
A: Continue to see the person and not the condition. Continue to support the person and not the condition. Continue to give life to the person and not the condition. The person is still there. They might look a little different. They might sound a little different. They might even think and process a little differently. But they’re still there. See them for who they are today, not yesterday.
RELATED POSTS:
Geriatric Specialist’s Practical Guidance on Caring for Loved Ones with Dementia
 Dr. Macie Smith is an award-winning educator with 19 years of experience working with aging and vulnerable populations in South Carolina. She is the acting President of the National Association of Social Workers-South Carolina Chapter. Dr. Smith is a Licensed Social Worker, Certified Social Work Case Manager, and a Social Worker in Gerontology who provides private Geriatric Care Management to families living with dementia. She also serves as Professor and a Subject Matter Expert on the collegiate level in the areas of social work, social sciences and public health at the University of South Carolina and the University of Phoenix. Dr. Smith conducts research and facilitates professional development training in the areas of health care management, human services development and program development. Her focus is coordinating quality care within aging and underserved communities. Dr. Smith has been recognized as a Top 20 Under 40 Leader by the South Carolina Black Pages Magazine for her work as a community and industry change agent.
Dr. Macie Smith is an award-winning educator with 19 years of experience working with aging and vulnerable populations in South Carolina. She is the acting President of the National Association of Social Workers-South Carolina Chapter. Dr. Smith is a Licensed Social Worker, Certified Social Work Case Manager, and a Social Worker in Gerontology who provides private Geriatric Care Management to families living with dementia. She also serves as Professor and a Subject Matter Expert on the collegiate level in the areas of social work, social sciences and public health at the University of South Carolina and the University of Phoenix. Dr. Smith conducts research and facilitates professional development training in the areas of health care management, human services development and program development. Her focus is coordinating quality care within aging and underserved communities. Dr. Smith has been recognized as a Top 20 Under 40 Leader by the South Carolina Black Pages Magazine for her work as a community and industry change agent.
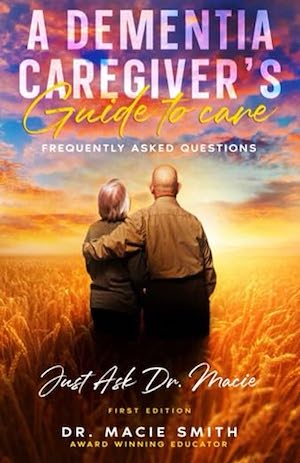
Publish Date: February 14, 2019
Genre: Nonfiction
Author: Macie Smith
Page Count: 73 pages
ISBN: 9798378150205

























:quality(85):upscale()/2025/05/23/715/n/1922564/1e63d6e168309df259d956.72331408_.png)

:quality(85):upscale()/2025/05/06/835/n/1922564/8e601b95681a5cf04194c6.14070357_.png)